Our bodies are complex systems where mental and physical health are deeply intertwined. Recent studies highlight how psychological stress, such as manipulation, can disrupt the delicate balance between the gut and the brain axis. This disruption often leads to physical symptoms, including digestive issues like irritable bowel syndrome.
Research shows that emotional distress can alter the gut microbiome, the community of microorganisms in our digestive system. These changes can affect not only digestion but also mood and overall well-being. Understanding this connection helps us recognize the importance of mental health in maintaining physical health.
Key Takeaways
- Psychological stress can disrupt the gut-brain connection.
- Changes in the gut microbiome may lead to digestive issues.
- Emotional health plays a key role in physical well-being.
- Understanding this link can improve treatment approaches.
- Mental health care is essential for overall health.
Introduction to the Gut-Brain Axis
Modern science reveals a fascinating dialogue between our digestive system and our mind. This connection, often referred to as the gut-brain axis, plays a critical role in our overall health. It’s not just about hunger signals—this axis influences mood, cognitive function, and even disease prevention.
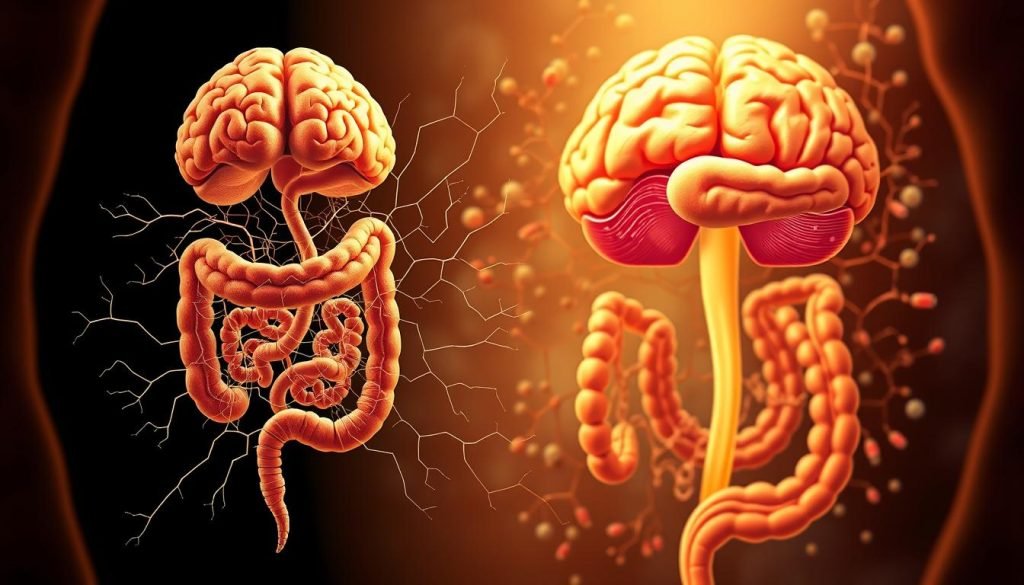
Definition and Significance
The gut-brain axis is a two-way communication system linking the digestive tract and the central nervous system. It involves neural, hormonal, and immunological pathways. This connection is vital because it helps regulate everything from digestion to emotional well-being.
For example, an imbalance in gut bacteria can lead to conditions like irritable bowel syndrome. Similarly, stress or anxiety can disrupt digestion, showing how closely the gut and brain are intertwined.
Communication Pathways Between Gut and Brain
Several key pathways facilitate this communication. The vagus nerve, often called the “wandering nerve,” is a major neural link. It carries signals from the gut to the brain and vice versa. Hormones like serotonin, which is primarily produced in the gut, also play a role.
Additionally, the immune system contributes to this dialogue. Inflammation in the gut can trigger responses in the brain, potentially leading to mental health issues. Understanding these pathways is essential for addressing both physical and mental disease.
Recognizing this connection can help us take better care of our health. For instance, improving gut health through diet or probiotics may alleviate symptoms of anxiety or depression. Similarly, managing stress can support digestive health. If you’re navigating challenges like toxic relationships, understanding this link can be a step toward healing.
The Impact of Gaslighting on Our Health
Psychological manipulation leaves more than just emotional scars—it can deeply affect our physical health. Gaslighting, a form of emotional abuse, often goes unnoticed but can disrupt our bodily functions, particularly in the gut. This subtle yet harmful behavior can lead to long-term health issues, including digestive problems like irritable bowel syndrome.
Prolonged exposure to gaslighting can disturb the balance of our microbiome, the community of microorganisms in our digestive system. Stress from emotional abuse alters this delicate ecosystem, leading to symptoms such as bloating, diarrhea, and constipation. These changes not only affect digestion but also influence mood and overall well-being.
Understanding Gaslighting Behavior
Gaslighting is a manipulative tactic that makes individuals doubt their reality. This psychological stress can trigger physical responses, particularly in the gut. Research shows that emotional abuse is strongly linked to shifts in gut health, including conditions like irritable bowel syndrome.
For example, chronic stress from gaslighting can increase inflammation in the gut, disrupting its normal function. This inflammation can further affect the microbiome, creating a cycle of discomfort and health issues. Understanding this connection helps us recognize the importance of addressing emotional abuse for both mental and physical health.
Here’s a breakdown of how gaslighting impacts gut health:
| Effect | Description |
|---|---|
| Stress Response | Triggers inflammation in the gut, disrupting the microbiome. |
| Digestive Issues | Leads to symptoms like bloating, diarrhea, and constipation. |
| Mood Changes | Alters neurotransmitter production, affecting emotional well-being. |
Empirical evidence supports the link between emotional abuse and gut health. A 2018 study found that adverse childhood experiences, including emotional abuse, could increase the risk of chronic pain conditions and digestive disorders. Similarly, unresolved trauma has been linked to a higher prevalence of irritable bowel syndrome.
Addressing gaslighting and its effects requires a holistic approach. This includes recognizing the signs of emotional abuse, seeking support, and taking steps to restore gut health. For more on recognizing harmful behaviors, explore our guide on workplace harassment.
Exploring Gut-brain axis dysregulation from gaslighting
Stress from manipulation can trigger a cascade of changes in the gut, affecting both physical and mental well-being. These changes are driven by biological and neurological mechanisms that link emotional stress to digestive health. Understanding these processes helps us address the root causes of related symptoms.
Mechanisms Behind the Dysregulation
Emotional stress, such as that caused by manipulation, can alter the balance of gut bacteria. This imbalance disrupts the gut’s ability to function properly, leading to symptoms like bloating, diarrhea, and constipation. Studies show that stress-induced changes in the microbiome can also impact mood and cognitive function.
One key mechanism involves the production of biologically active substances in the gut. These substances, including neurotransmitters like serotonin, play a crucial role in brain function. When stress disrupts this process, it can lead to a range of physical and mental health issues.
Research highlights the importance of maintaining a balanced microbiome for proper gut-brain communication. For example, a 2018 study found that chronic stress can increase inflammation in the gut, further disrupting its function. This inflammation can create a cycle of discomfort and health problems.
Here’s how stress affects the gut-brain connection:
- Alters gut bacteria, leading to digestive symptoms.
- Disrupts neurotransmitter production, affecting mood.
- Increases inflammation, contributing to chronic health issues.
Addressing these mechanisms requires a holistic approach. This includes managing stress, improving gut health through diet, and seeking support for emotional well-being. By understanding these connections, we can take steps to restore balance and improve overall health.
The Enteric Nervous System and Vagus Nerve Connection
The enteric nervous system, often called the “second brain,” plays a pivotal role in our digestive health. This intricate network of neurons operates within the gastrointestinal tract, controlling digestion and nutrient absorption. It works independently but remains closely connected to the central nervous system, forming a vital link in our overall well-being.
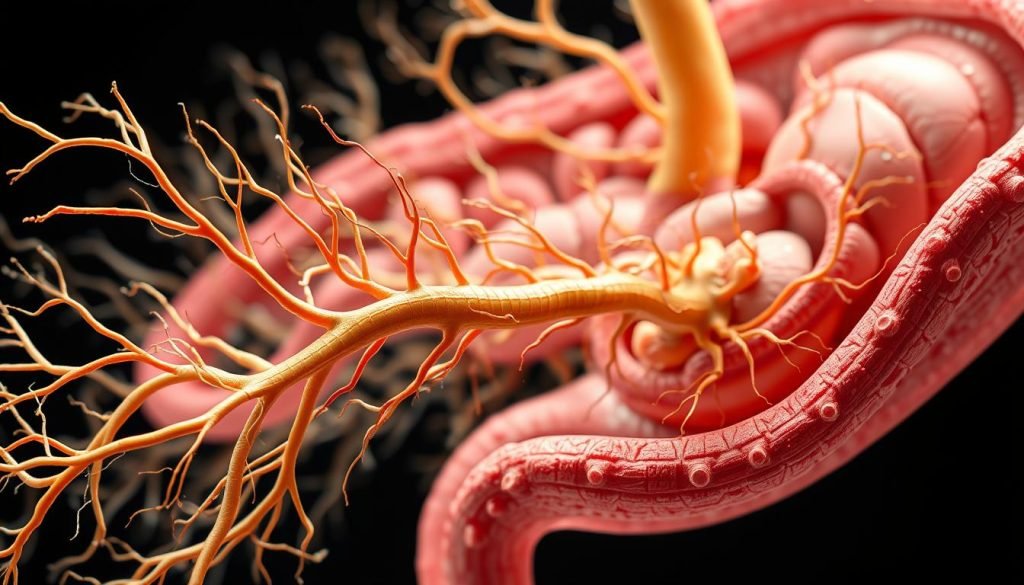
Overview of the Enteric Nervous System
The enteric nervous system is a complex neural network embedded in the walls of the gut. It regulates essential digestive functions, such as motility and enzyme secretion. Often referred to as the “second brain,” it can operate autonomously but communicates with the brain through the vagus nerve.
This system is crucial for maintaining digestive balance. When it functions properly, it ensures efficient digestion and nutrient absorption. However, disruptions can lead to issues like bloating, constipation, or even more severe conditions such as irritable bowel syndrome.
Role of the Vagus Nerve in Communication
The vagus nerve serves as the primary communication channel between the gut and the brain. It transmits signals in both directions, influencing everything from digestion to mood. For example, gut signals can impact emotions, while stress can disrupt digestive processes.
Research shows that the vagus nerve plays a key role in moderating anxiety and other emotional responses. When this nerve functions optimally, it helps maintain a balanced gut-brain connection. Conversely, dysfunction can contribute to disorders like chronic stress or digestive issues.
Understanding this connection is essential for addressing both physical and mental health. For those struggling with emotional challenges, such as anxious attachment styles, recognizing the role of the vagus nerve can be a step toward healing.
Effects on Mental Health: Anxiety, Depression, and Stress
Mental health challenges like anxiety and depression are deeply connected to our digestive system. Research shows that an imbalance in gut bacteria can significantly impact our emotional well-being. This connection highlights the importance of maintaining a healthy gut for both physical and mental health.
Chronic stress plays a major role in disrupting this balance. When stress levels rise, the body produces more cortisol, a hormone that can harm the gut lining. This can lead to digestive issues and further exacerbate mental health problems. Studies suggest that managing stress is key to maintaining a healthy gut and stable mood.

A balanced diet is another critical factor. Foods rich in fiber and probiotics support a diverse gut microbiome, which in turn helps regulate mood and reduce anxiety. For example, prebiotic fiber is converted into short-chain fatty acids, which modulate neurotransmitter levels in the brain. This process can alleviate symptoms of anxiety and depression.
Here’s a summary of how gut health impacts mental well-being:
| Factor | Impact |
|---|---|
| Chronic Stress | Increases cortisol, harming gut lining and mental health. |
| Balanced Diet | Supports gut bacteria, improving mood and reducing anxiety. |
| Gut Bacteria | Produces serotonin, a key neurotransmitter for emotional stability. |
Empirical evidence supports these connections. For instance, a 2022 study found that specific gut metabolites can influence anxious behavior. Similarly, chronic stress has been linked to systemic inflammation, which increases the risk of depression. By understanding these links, we can take proactive steps to improve both gut and mental health.
Taking care of our digestive system is not just about physical well-being—it’s a vital part of maintaining emotional balance. Simple changes, like reducing stress and eating a nutrient-rich diet, can make a significant difference. Let’s prioritize our gut health to support a happier, healthier mind.
The Gut Microbiome’s Role in Brain Function
The trillions of microbes in our gut are key players in brain health and emotional stability. These microorganisms, collectively known as the microbiome, produce or assist in producing neurotransmitters that facilitate communication between the gut and brain. This process is essential for maintaining both mental and physical well-being.
Linking Microbiota to Neurotransmitter Production
Our gut microbes play a crucial role in synthesizing neurotransmitters like serotonin and dopamine. These chemicals are vital for regulating mood, cognition, and emotional responses. For example, nearly 90% of serotonin, a neurotransmitter linked to happiness, is produced in the gut.
When the microbiome is balanced, it supports optimal brain function. However, disruptions can lead to imbalances in neurotransmitter levels, contributing to conditions like anxiety and depression. Research shows that maintaining a healthy gut microbiome is key to emotional stability.
Inflammatory Responses and Immune System Links
The microbiome also influences inflammation and immune responses. A healthy gut can reduce inflammation, while an imbalanced microbiome may trigger chronic inflammation. This inflammation can affect the brain, leading to cognitive and emotional challenges.
For instance, studies have linked gut inflammation to conditions like irritable bowel syndrome and even depression. The immune system plays a dual role here, both protecting the body and potentially exacerbating inflammation when the microbiome is disrupted.
Here’s a summary of the gut microbiome’s impact:
| Aspect | Effect |
|---|---|
| Neurotransmitter Production | Supports mood and cognitive function. |
| Inflammation | Can reduce or trigger systemic inflammation. |
| Immune Response | Modulates immune system activity. |
Understanding these connections helps us appreciate the importance of gut health. By supporting our microbiome through diet and lifestyle, we can enhance both mental and physical well-being.
Understanding IBS and Bowel Syndrome in Context
Irritable bowel syndrome (IBS) is a common yet complex condition that affects millions of people worldwide. It’s characterized by chronic abdominal pain, bloating, and changes in bowel habits. These symptoms often disrupt daily life, making it essential to understand the condition within the broader context of digestive health.
One of the key factors in managing IBS is maintaining healthy bowel function. A diet rich in fiber plays a crucial role in this process. Fiber helps regulate digestion, preventing both constipation and diarrhea, which are common symptoms of IBS. Including whole grains, fruits, and vegetables in your diet can significantly improve bowel health.
Stress and diet are major contributors to IBS and other bowel syndromes. Chronic stress can disrupt the digestive system, leading to symptoms like cramping and irregular bowel movements. Similarly, certain foods, such as those high in fat or processed sugars, can exacerbate these issues. Understanding these triggers is vital for effective management.
Here’s a breakdown of how IBS differs from other digestive disorders:
- IBS involves chronic abdominal pain linked to bowel movements.
- It’s often accompanied by bloating and changes in stool consistency.
- Unlike inflammatory bowel disease, IBS doesn’t cause structural damage to the gut.
The interactions between bowel function and the nervous system are also critical. The enteric nervous system, often called the “second brain,” communicates with the central nervous system to regulate digestion. When this communication is disrupted, it can lead to symptoms of IBS.
Recognizing IBS early can lead to more effective management strategies. Lifestyle changes, such as increasing fiber intake and reducing stress, can make a significant difference. For those struggling with symptoms, consulting a healthcare professional is essential for a tailored treatment plan.
By understanding the complexities of IBS and its impact on bowel function, we can take proactive steps to improve digestive health and overall well-being.
How Diet and Stress Influence Gut Functioning
The foods we eat and the stress we experience play a significant role in how our digestive system functions. Both diet and stress can either support or disrupt the delicate balance of our gut microbiome, leading to various health challenges. Understanding these factors helps us make informed choices for better digestive health.
Impact of Fiber and Processed Foods
A diet rich in fiber is essential for maintaining a healthy gut. Fiber acts as fuel for beneficial gut bacteria, promoting a balanced microbiome. Foods like whole grains, fruits, and vegetables are excellent sources of fiber. On the other hand, processed foods high in sugar and unhealthy fats can harm gut health by reducing microbial diversity.
Research shows that diets high in processed foods can increase inflammation levels in the gut. This inflammation disrupts digestive processes and can lead to conditions like irritable bowel syndrome. For each person, adopting a fiber-rich diet can make a significant difference in gut health.
Stress, Cortisol, and Gut Health
Chronic stress triggers the release of cortisol, a hormone that can negatively impact the gut. Elevated cortisol levels disrupt the gut lining, increasing permeability and inflammation. This can lead to symptoms like bloating, cramping, and irregular bowel movements.
Studies indicate that stress-induced cortisol spikes can alter the gut microbiome, reducing the presence of beneficial bacteria. Over time, this imbalance can affect both digestive and mental health. Managing stress through mindfulness, exercise, and relaxation techniques is crucial for maintaining gut health.
Here’s a summary of how diet and stress influence gut functioning:
| Factor | Impact on Gut Health |
|---|---|
| High-Fiber Diet | Supports beneficial bacteria and reduces inflammation. |
| Processed Foods | Increases inflammation and disrupts microbial balance. |
| Chronic Stress | td>Elevates cortisol, harming the gut lining and microbiome.
By prioritizing a balanced diet and effective stress management, we can support our gut health and overall well-being. Small changes, like adding more fiber-rich foods and practicing relaxation techniques, can have a lasting positive impact.
Recent Scientific Research and Key Studies
Scientific advancements have shed light on the intricate relationship between our gut and brain. Over the past decade, landmark studies have deepened our understanding of how the gut microbiome influences both physical and mental health. These findings have paved the way for innovative treatments and a more holistic approach to health care.

Landmark Studies on Gut-Brain Communication
One of the most significant breakthroughs came from studies focusing on the vagus nerve. This critical pathway connects the gut and brain, enabling bidirectional communication. Research has shown that disruptions in this nerve can lead to various health conditions, including digestive disorders and mood imbalances.
Another pivotal study explored how stress-induced changes in the gut microbiome affect mental health. Chronic stress alters the balance of gut bacteria, leading to symptoms like anxiety and depression. These findings emphasize the importance of managing stress for overall well-being.
Emerging Trends in Gut Research
Recent research is uncovering new links between gut health and neurological conditions. For example, studies suggest that an imbalanced microbiome may contribute to conditions like Parkinson’s disease and Alzheimer’s. This has led to a shift in focus toward integrative approaches that combine diet, probiotics, and lifestyle changes.
Innovative methods, such as advanced imaging and microbiome analysis, are also transforming how we study gut-brain communication. These tools allow researchers to observe real-time changes in the gut and their impact on the brain.
As we continue to explore these connections, it’s clear that addressing gut health is essential for preventing and managing a wide range of conditions. For those navigating challenges like toxic relationships, understanding this link can be a step toward healing.
Treatment Approaches: Probiotics and Omega-3 Supplements
Emerging treatments like probiotics and omega-3 supplements are transforming how we approach gut health. These dietary supplements have shown promise in reducing inflammation and restoring microbial balance in the digestive tract. By addressing the root causes of gut imbalances, they offer a holistic way to improve both physical and mental well-being.
Benefits of Probiotics on Inflammation
Probiotics, often referred to as “good bacteria,” play a crucial role in maintaining gut health. Studies have shown that they can reduce inflammatory cytokines, which are molecules that contribute to chronic inflammation. This reduction helps restore the balance of the gut microbiome, promoting better digestion and overall health.
For example, a 2022 study found that probiotics significantly lowered inflammation markers in participants with digestive issues. This highlights their potential as a treatment for conditions like irritable bowel syndrome. By supporting the gut-brain connection, probiotics also contribute to improved mood and reduced stress levels.
Role of Omega-3 in Maintaining Gut Health
Omega-3 fatty acids, commonly found in fish oil, are another powerful tool for gut health. They have been shown to beneficially affect the composition of gut microbiota, reducing systemic inflammation. This makes them particularly effective in managing conditions linked to chronic inflammation, such as depression and anxiety.
Research indicates that omega-3s can improve the gut-brain axis by enhancing communication between the digestive system and the brain. A 2021 study demonstrated that participants who took omega-3 supplements experienced fewer digestive symptoms and reported better mental clarity. This underscores their role in promoting both physical and emotional well-being.
Integrative treatment approaches that combine probiotics and omega-3s are essential for managing gut dysregulation caused by stress or emotional challenges. By addressing both inflammation and microbial balance, these supplements offer a comprehensive solution for improving gut health and overall quality of life.
Investigating Leaky Gut Syndrome and Systemic Effects
Leaky gut syndrome is a condition where the intestinal lining becomes more permeable, allowing harmful substances to enter the bloodstream. This condition often develops due to imbalances in digestion caused by an unhealthy diet or chronic stress. When the gut lining is compromised, it can lead to widespread inflammation and other systemic issues.
The systemic effects of a leaky gut are far-reaching. Inflammation triggered by this condition can disrupt the nervous system, leading to symptoms like fatigue, brain fog, and mood disorders. Research suggests that an impaired vagus nerve function may exacerbate these effects, as this nerve plays a critical role in gut-brain communication.
Clinical studies highlight the cascade of adverse effects from a compromised intestinal barrier. For instance, a 2020 study found that individuals with leaky gut syndrome were more likely to experience autoimmune conditions and chronic inflammation. Early diagnosis and dietary intervention are crucial to prevent further systemic dysfunction.
Understanding the interconnectedness of digestion issues and overall nervous system health is essential. By addressing the root causes of leaky gut, such as poor diet and stress, we can take proactive steps to restore balance and improve well-being.
Neurotransmitters and Hormonal Signaling Along the Axis
The gut is a powerhouse of chemical activity, producing neurotransmitters and hormones that influence our mood and mental health. These chemicals play a vital role in maintaining emotional balance and overall well-being. Understanding how they function helps us appreciate the intricate connection between our digestive system and brain.
Serotonin, GABA, and Other Neurochemicals
Serotonin, often called the “feel-good” neurotransmitter, is primarily produced in the gut. It regulates mood, appetite, and sleep. Similarly, GABA, a calming neurotransmitter, helps reduce anxiety and stress. Both are synthesized by gut bacteria, highlighting the importance of a healthy gut microbiome.
Imbalances in these neurochemicals can lead to mental health issues like depression and anxiety. For example, low serotonin levels are linked to mood disorders, while insufficient GABA can cause heightened stress responses. Maintaining a balanced gut environment is essential for stable neurotransmitter production.
Here’s a summary of key neurotransmitters and their roles:
| Neurotransmitter | Role |
|---|---|
| Serotonin | Regulates mood, appetite, and sleep. |
| GABA | Reduces anxiety and promotes relaxation. |
| Dopamine | Influences motivation and reward systems. |
Hormonal signaling also plays a crucial role. Hormones like ghrelin and leptin, produced in the gut, regulate hunger and energy balance. Disruptions in these signals can affect both physical and mental health. For instance, irregular ghrelin levels may lead to overeating, which can exacerbate mood disorders.
Research shows that the gut microbiome composition directly impacts neurotransmitter production. A diverse microbiome supports optimal chemical balance, while imbalances can trigger symptoms of depression and anxiety. This underscores the need for a healthy gut to maintain emotional stability.
By understanding these connections, we can take proactive steps to support our gut and brain health. For those navigating challenges like toxic relationships, focusing on gut health can be a key part of the healing process.
Integrative Approaches to Treatment and Therapy
Combining dietary changes with behavioral therapies offers a holistic way to improve gut and mental health. Recent articles highlight the effectiveness of integrative strategies in addressing gut dysregulation. These approaches focus on restoring balance through food choices and therapeutic interventions.
Dietary Modifications for Better Gut Health
A nutrient-rich diet is essential for maintaining a healthy gut. Whole foods like fruits, vegetables, and whole grains provide the fiber needed to support beneficial bacteria. Processed foods, on the other hand, can disrupt the gut microbiome and lead to inflammation.
Studies show that diets rich in probiotics and prebiotics can improve gut health. Probiotics introduce beneficial bacteria, while prebiotics act as fuel for these microbes. Including fermented foods like yogurt and sauerkraut in your diet can make a significant difference.
Behavioral and Therapeutic Interventions
Therapeutic approaches like cognitive-behavioral therapy (CBT) can support gut health by reducing stress. Chronic stress disrupts the gut-brain connection, leading to digestive issues. CBT helps individuals manage stress, which in turn supports a balanced gut microbiome.
Mindfulness practices, such as meditation and deep breathing, also play a role. These techniques reduce cortisol levels, promoting a healthier gut environment. For those seeking a comprehensive approach, combining these therapies with dietary changes can yield the best results.
Here’s a summary of key practices for improving gut health:
| Practice | Benefit |
|---|---|
| Whole Foods Diet | Supports beneficial bacteria and reduces inflammation. |
| Probiotic Supplements | Introduces beneficial bacteria to the gut. |
| Mindfulness Practices | Reduces stress and supports gut-brain balance. |
For those navigating challenges like trauma, an integrative approach to healing can be transformative. By addressing both dietary and emotional needs, we can restore balance and improve overall well-being.
The Evolution of Our Understanding of the Gut-Brain Axis
The journey to understanding the gut-brain relationship has been marked by groundbreaking discoveries. Over the years, our comprehension of this connection has evolved from early observations to advanced scientific research. This evolution has reshaped the way we approach health and wellness.
Initially, the gut was seen merely as a digestive organ. However, studies revealed its role in influencing mood and behavior. The discovery of the microbiota as a key player in this process was a turning point. Today, we recognize that these microorganisms are essential for maintaining balance in the body.
One of the most significant shifts in perception has been the link between gut signals and chronic pain. Research shows that imbalances in the gut can trigger inflammatory responses, leading to discomfort. This understanding has paved the way for innovative treatments targeting the gut to alleviate pain.
Key breakthroughs have also redefined our approach to managing gut-related disorders. For instance, the identification of the vagus nerve as a communication pathway between the gut and brain has been transformative. This discovery has led to therapies that focus on restoring this connection.
Here’s a summary of pivotal milestones in gut-brain research:
| Milestone | Impact |
|---|---|
| Discovery of Microbiota | Highlighted the role of gut bacteria in health. |
| Vagus Nerve Research | Uncovered the neural link between gut and brain. |
| Chronic Pain Studies | Linked gut imbalances to inflammatory responses. |
These advancements guide the way we approach diagnosis and therapy today. By understanding the gut-brain connection, we can develop more effective treatments. This holistic approach ensures that both physical and mental health are addressed.
As we continue to explore this field, it’s clear that the gut-brain relationship holds the key to unlocking new possibilities in healthcare. The evolution of our understanding has not only deepened our knowledge but also improved the way we care for our well-being.
Practical Steps We Can Take to Restore Balance
Restoring balance to our body and mind requires intentional steps and mindful practices. By focusing on lifestyle changes and self-care, we can improve both our physical and emotional well-being. Let’s explore actionable strategies to achieve this balance.
Lifestyle Changes and Self-care
Improving sleep patterns is a foundational step. Quality sleep helps regulate stress hormones and supports overall health. Aim for 7-9 hours of restful sleep each night by creating a calming bedtime routine.
Stress management techniques, such as mindfulness and meditation, can also make a significant difference. These practices reduce cortisol levels, promoting a healthier gut and mind. Regular physical activity, like yoga or walking, further enhances this effect.
Diet adjustments are equally important. Incorporate foods rich in fiber and probiotics to support gut health. Avoid processed foods and sugary drinks, which can increase inflammation. For example, fermented foods like yogurt and kimchi introduce beneficial bacteria to the gut.
Consulting Healthcare Professionals
While self-care is essential, professional guidance ensures a comprehensive approach. Consulting a healthcare provider can help identify underlying issues and tailor a plan to your needs. Therapy, for instance, can address emotional challenges that impact physical health.
Behavioral changes, such as setting boundaries and managing stress, are often more effective with professional support. For those navigating challenges like leaving a toxic relationship, therapy provides tools for healing and growth.
Here’s a summary of key practices to restore balance:
| Practice | Benefit |
|---|---|
| Improved Sleep | Reduces stress hormones and supports overall health. |
| Mindfulness | Lowers cortisol levels, promoting gut-brain balance. |
| Diet Adjustments | Supports gut health and reduces inflammation. |
| Professional Therapy | Addresses emotional challenges and provides tailored guidance. |
By combining these strategies, we can take meaningful steps toward restoring balance and improving our quality of life. Remember, small changes can lead to significant results when approached consistently and with care.
Conclusion
Understanding the connection between our digestive system and mental health is key to overall wellness. Emotional stress can disrupt this balance, affecting both the immune system and the vagus nerve, which play crucial roles in maintaining harmony between the gut and brain.
Scientific research continues to highlight the importance of this relationship. Integrative treatments, such as dietary changes and stress management, offer effective ways to restore balance. By addressing both physical and emotional health, we can improve our quality of life.
We encourage readers to explore therapies that support the vagus nerve and strengthen the immune system. Consulting healthcare professionals ensures personalized care and effective solutions. Together, we can take meaningful steps toward better health and well-being.
Source Links
- Feeling Depressed? Gut-Brain Dysfunction May Be to Blame – https://www.psychologytoday.com/intl/blog/the-mindful-self-express/201812/feeling-depressed-gut-brain-dysfunction-may-be-blame
- The Intricate Relationship of the Brain-Gut Axis – CARAVAN Wellness – https://blog.caravanwellness.com/the-intricate-relationship-of-the-brain-gut-axis/
- RHR: Understanding the Connection Between What You Eat and How You Feel, with Dr. Will Cole – https://chriskresser.com/understanding-the-connection-between-what-you-eat-and-how-you-feel-with-dr-will-cole/
- Targeting the Gut in the Treatment of Mental Illness – https://www.psychologytoday.com/intl/blog/balanced/202308/targeting-the-gut-in-the-treatment-of-mental-illness
- The Vagus Nerve May Carry Serotonin Along the Gut-Brain Axis – https://www.psychologytoday.com/intl/blog/the-athletes-way/201910/the-vagus-nerve-may-carry-serotonin-along-the-gut-brain-axis
- Parenting Series | Expressive Trauma In – https://www.eti.training/parenting-series
- Effects of Emotional Abuse on Your Brain, Relationships, and Health – https://psychcentral.com/health/effects-of-emotional-abuse
- Understanding The Mind-Body Connection – https://drwillcole.com/mindful-living/mind-body-connection
- Finding Safety to Heal: The Gut-Brain Connection and Releasing Trapped Emotions – (IN)tentionally Rooted In Healing – https://intentionallyrootedinhealing.buzzsprout.com/2432156/episodes/16251856-finding-safety-to-heal-the-gut-brain-connection-and-releasing-trapped-emotions
- Frontiers | Dysautonomia following Lyme disease: a key component of post-treatment Lyme disease syndrome? – https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2024.1344862/full
- 9 Tips for Improving the Gut–Brain Connection – https://www.psychologytoday.com/intl/blog/the-binge-eating-prevention-plan/202304/9-tips-for-improving-the-gut-brain-connection
- Connecting the Dots: Ruhoy and Kaufman Take on Connective Tissues in ME/CFS, Fibromyalgia and Long COVID – Health Rising – https://www.healthrising.org/blog/2024/04/22/connective-tissue-chronic-fatigue-long-covid-fibromyalgia/
- Martin’s Paradoxical Temporary ME/CFS Remission Story – Health Rising – https://www.healthrising.org/blog/2024/07/31/martin-chronic-fatigue-syndrome-remission/
- Exploring the Link Between the Gut Microbiome and Anxiety – https://www.psychologytoday.com/intl/blog/the-resilient-brain/202307/exploring-the-link-between-the-gut-microbiome-and-anxiety
- How Brain Inflammation Affects Your Mental Health and Decision-Making | Dr. Austin Perlmutter – https://drbrighten.com/podcasts/how-brain-inflammation-affects-your-mental-health/
- The Gut-Brain Axis Unveiled: Exploring its Impact on Depression. Kiran Krishnan with Microbiome Labs-Heather Gray FDN-P by Renegade Health Boss: Health Transformations using Functional health for Lyme & Autoimmune Disease – https://creators.spotify.com/pod/show/lymebossheathergray/episodes/The-Gut-Brain-Axis-Unveiled-Exploring-its-Impact-on-Depression–Kiran-Krishnan-with-Microbiome-Labs-e267j2i
- Why doctors are ignorant and dismissive of the gut-brain relationship | Aeon Essays – https://aeon.co/essays/why-doctors-are-ignorant-and-dismissive-of-the-gut-brain-relationship
- Stress Eating and the Microbiome – https://www.psychologytoday.com/intl/blog/mood-by-microbe/202502/stress-eating-and-the-microbiome
- The key to gut health is a regulated nervous system — Gutivate – https://gutivate.com/blog/regulated-nervous-system
- Dysregulation of Dopamine in the Brain Indicates Multiple Neurological & Mental Health Conditions – https://medium.com/illumination/dysregulation-of-dopamine-in-the-brain-indicates-multiple-neurological-mental-health-conditions-fc8b7da12cb4
- Frontiers | Outdoor nighttime light exposure (light pollution) is associated with Alzheimer’s disease – https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1378498/full
- Long COVID Brain Fog: Why it Happens & How to Recover – Dr. Michael Ruscio, DC – https://drruscio.com/long-covid-brain-fog/
- Podcast | Ali Miller RD – https://www.naturallynourishedrd.com/podcast/
- Digesting the Facts: Tackling Gastrointestinal Challenges in EDS – EDSAwareness.com – https://www.chronicpainpartners.com/digesting-the-facts-tackling-gastrointestinal-challenges-in-eds/
- PDF – https://pure.uva.nl/ws/files/220595692/Chapter_10.pdf
- CRPS Primer – CRPScontender – https://crpscontender.com/index.php/crps-primer/
- Where Sex Meets Gender: How Sex and Gender Come Together to Cause Sex Differences in Mental Illness – https://www.frontiersin.org/articles/10.3389/fpsyt.2022.856436/pdf
- Breaking Free from Binge Eating and Digestive Issues Through The Magic of Herbs | Stephanie Mara – https://www.stephaniemara.com/blog/breaking-free-from-binge-eating-and-digestive-issues
- Depression, the Gut Microbiome, and Vitamins – https://www.psychologytoday.com/intl/blog/advancing-psychiatry/202405/depression-the-gut-microbiome-and-vitamins
- IMMH: Integrative Medicine for Mental Health Course – https://catalog.pesi.com/sales/hc_c_001787_immhcourse_organic-778929
- Lyme Disease + Mental Health: Ways to Improve It from a Lyme-Literate Therapist | RawlsMD – https://rawlsmd.com/health-articles/lyme-disease-mental-health-ways-to-improve-it-from-a-lyme-literate-therapist
- ADHD Expert Webinars & Podcast Episodes – Index by Date + Slides – https://www.additudemag.com/adhd-expert-webinars-index/?srsltid=AfmBOor1MM0svGF1L4ETii7ENNdrKyKq2BEb3v8K9FnliGYkeTWiBbiq
- Eye Movement Therapy, the Vagus Nerve, and Polyvagal Theory – https://integraleyemovementtherapy.com/eye-movement-therapy-the-vagus-nerve-and-polyvagal-theory/
- How Inflammation Can Threaten Your Mental Health – https://www.psychologytoday.com/us/blog/the-modern-brain/202412/how-inflammation-affects-your-mental-health
- 6 Promising Signs Your Body is Releasing Trauma – https://therapistsinphiladelphia.com/blog/signs-your-body-is-releasing-trauma/
- Endometriosis and The Pain of Medical Gaslighting with Endometriosis Surgeon, Dr. Madhu Bagaria, MD, FACOG – https://integrativewomenshealthinstitute.com/endometriosis-and-the-pain-of-medical-gaslighting-with-endometriosis-surgeon-dr-madhu-bagaria-md-facog/
- Gut bacteria and ocd – https://thewrightinitiative.com/misc/gut-bacteria-and-ocd.html

Amanda Cassey is an INTJ entrepreneur and former psychology researcher who writes about the nuances of the INTJ personality type on Psyche Central. Leveraging her analytical mindset and commitment to personal growth, she explores the cognitive processes, strengths, and challenges of INTJs. Her insightful content aims to foster self-awareness and provide practical strategies for fellow INTJs to thrive.

Leave a Reply